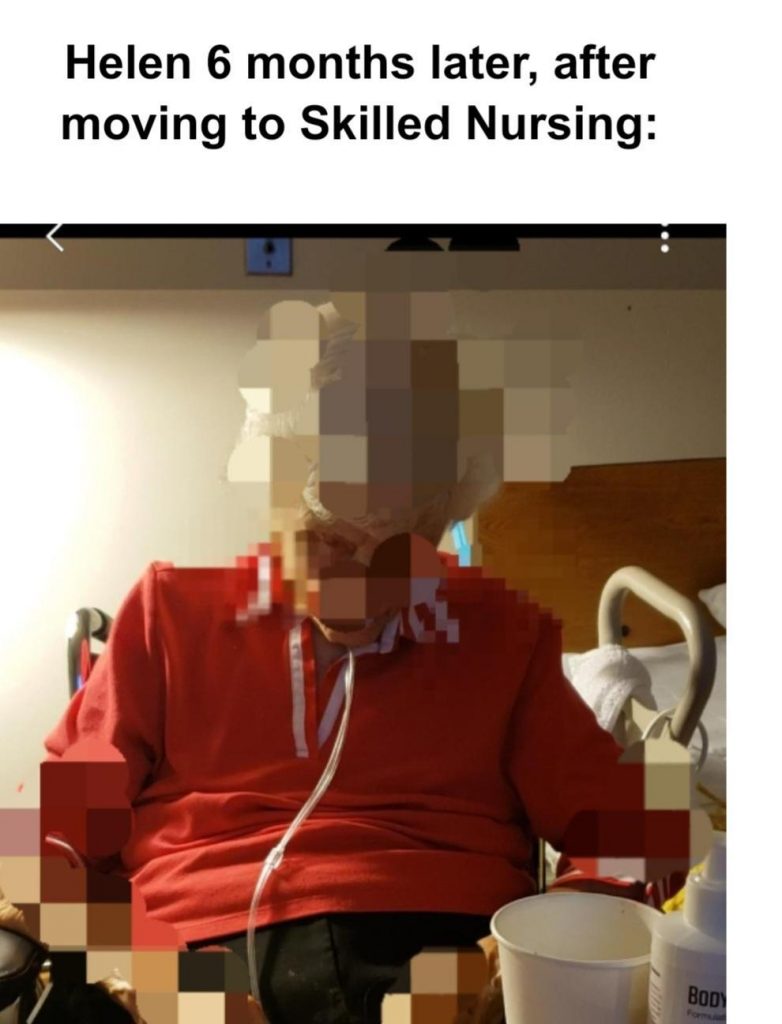
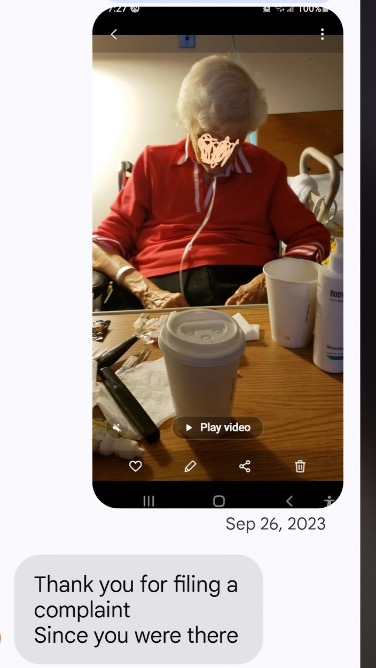
Helen asleep in her wheelchair while waiting for an hour after asking for help with going to bed. She slept another 30 minutes before anyone came to help her. It had happened the week before also. The charge nurse had given her a sleeping pill 90 minutes earlier and the staff just left her to fall asleep in her wheelchair. I stifled my anger and said, She’s been waiting an hour-and-a-half.
The charge nurse shrugged her shoulders and replied, We were busy with other patients. This place felt like the twilight zone – like none of this abuse was any big deal! But it was a huge big deal!
Hospice services had begun and Helen was treated well by their staff. They spoke respectfully to her, listened patiently, and cared for her. But the care she received by the facility staff was abysmal. In desperation I called Adult Protective Services. They couldn’t help because it involved a nursing home. They gave me the phone number of the “State Ombudsman.” They couldn’t help because the facility was part of a retirement community – and gave me another phone number for a different Ombudsman. I decided to file a written report with documentation:
California Department of Social Services website:
If You SEE Something, SAY Something
“Phone: 844-LET US NO (844-538-8766)
Email: letusno@dss.ca.gov
Remember, when you report suspected violations, you not only protect individuals in care facilities, but also perform a service to your community.”
I was encouraged. The complaint was assigned to the Los Angeles County Public Health Department for investigation. I decided to submit the notes Helen had specifically asked me to write about – before things got worse and she became overwhelmed.
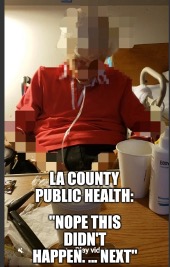
On October 19, 2023, an official from the Los Angeles County Department of Public Health [LACDPH] contacted me by phone to convey that the complaint was deemed “unsubstantiated,” and stated this meant “it didn’t happen.”
I was flabbergasted. Didn’t happen?
I was never interviewed by LACDPH staff. Instead, I initiated contact with the supervisor to provide additional information. The supervisor had his staff investigator call me and we discussed Helen’s lack of rights as a nursing home resident. These rights are a state and federal requirement and include providing her with a written copy of her rights – which the nursing facility never had done. This discussion lasted approximately five minutes. However, the staff member later claimed that our brief conversation was an interview. Yet, she hadn’t asked me a single question about the complaint and documentation I had submitted.
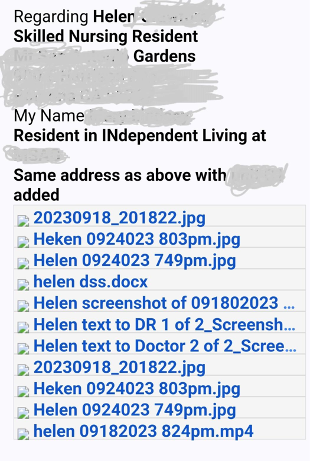
Below is the detailed complaint, and a list of attachments, that I submitted as documentation.
THE COMPLAINT And DOCUMENTATION submitted:
Allegation #1
Helen, resident in a skilled nursing home—100 years old, lived independently until July 2023, when she moved to skilled nursing. She recently chose to be placed on hospice services. Cognitively, she is still very aware and articulate – although she now speaks more slowly.
It’s difficult to have names (of staff) because sometimes staff are not wearing their ID and other times it is turned around so their name tag is facing away from patients. I used to visit at 8 pm and stay until 9:30 ish. But then they moved her bedtime to 7 pm so I began visiting at 6 pm and staying until she was asleep. The routine is very unpredictable and chaotic – creating high anxiety for Helen.
Allegation #2, 9/5/2023
Helen’s sleeping pill was withheld for hours. She was increasingly sleep deprived after being unable to sleep through the night and she was exhausted. They had told her she had to wait until 7 pm, so she watched the clock. At 7pm she asked for her sleeping pill and nurse Cold Fish told her no, she needed to wait until 9 pm or else she wouldn’t sleep until morning.
Helen begged her for the pill, but no, they made her wait. When I stepped out of the room while they got her ready for bed, the nurse came in and told Helen she would not give her a sleeping pill until after I had left for the evening.
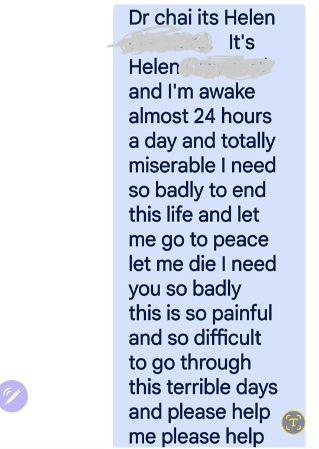
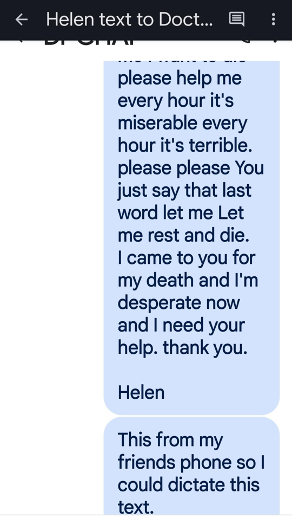
Helen then sent a desperate text message to her doctor – Dr. Chai – which I’ve included below.
Every 30 minutes she asked me what time it was. At 9:01, she asked me to leave and I did so immediately. But I waited at the end of the hall and the nurse did not appear for another 15 minutes after already making Helen wait for hours.
The next day, Helen told me that the nurse didn’t arrive for another 10 minutes after I’d left. (It was actually 15 minutes.) She then told me that the nurse told her that the pill she’d been giving Helen every night wasn’t a sleeping pill but something else. I suspected it was Ativan, which might help her get to sleep, but not stay asleep. That night, Helen didn’t sleep well.
Here is the heartbreaking text that Helen sent her doctor:
FINDING:
LACDPH and California Public Health Department [CPHD]:X_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
Allegation #3, September 6, 2023
Helen complained that evening to a male nurse/CNA that the pill wasn’t working. He explained that it took time to build up in her system – 4-6 weeks. This greatly upset Helen and made no sense to me. It turned out they were giving her an anti-depresssant, not a sleeping pill.
Allegation #4, September 7, 2023
They actually gave her a sleeping pill. It took an hour to take effect. Night after night I sat quietly with Helen, massaging and rubbing her swollen feet and ankles until she fell asleep. After a week she asked me if the pill had built up enough yet. I assured her it had. I think she was distressed every night because she had been told it would take 4-6 weeks before it would fully take effect. I realized that her anxiety might be getting in the way of her falling asleep.
X_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
Allegation #5, Sept 9, 2023
Helen was still tired during the day. We talked with the nurse, who told her she should be going to bed at 7 pm to get more sleep. She agreed and we all agreed she would go to bed at 7 pm – AFTER having her bedtime routine completed. In other words, she would be in bed BEFORE she was given her sleeping pill.
That evening, they gave her a sleeping pill at 7 pm and said someone would be there soon to get her ready for bed.
I had changed my schedule so I could come visit Helen earlier. Despite pushing the call button multiple times, we waited 20 to 30 minutes, each time, before someone told us that yes, someone would be coming to her room shortly. But, despite our explicit agreement, no one arrived for 90 minutes after she was given the pill and she had fallen asleep in her chair, her head slumped forward. (See attached photo/video)
The photo below is a print of the attached video submitted with the complaint:

X_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
Allegation #6, 9/16/2023
The nurse gave Helen her sleeping pill, which usually takes ~45 min to take effect, but this night she was “out like a light” in 12 minutes. nurse: L
X_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
Allegation #7 9/17/2023
Helen was very anxious and talked about “a bright yellow board” that they attached her to- to take her to the bathroom after waking her up (at 2 am.) She had asked what was happening and told “I don’t have time.” I thought it was because she may have been too sedated. During the day we asked Ethel (very kind) about the bright yellow board. She was puzzled and then exclaimed “You’re not supposed to be moved that way.” It turned out they had had a group of students performing these tasks – apparently without supervision.
Allegation #8 9/18/2023
After Helen had repeatedly asked to be included in decisions (about her care), and I had explained to facility staff that when she doesn’t know what’s going on she becomes very anxious, she waited all day for a shower but was not given one.
Rowland from the Hospice had told her when she signed up that they could do 2-3 showers a week and I clarified with him about whether these could be in addition to the two she received from the facility and he enthusiastically said “yes.” Until today she had been receiving 4 showers a week – two from the facility staff and two from the Hospice staff. Today, as Helen waited all day for her shower and did not receive one, she was told that the hospice person had not been able to come (she was out sick.) We asked if the hospice person would then come tomorrow to give her a shower. Nurse S (usually a very helpful and kind facility staff person, but today she was distant and business-like) informed Helen that she would no longer be receiving showers from the facility and only two showers a week from Charter. Helen was very upset. (It turned out Helen’s Medicare eligibility for nursing home services had run out. Now she was in the nursing facility under her prepaid fee contract she had paid for monthly for ovee 22 years – which apparently did not include two baths a week if she could receive these from another provider.)
X_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
Allegation #9, 9/20/23
When I arrived around 6 pm that evening, Helen was upset and asked me where I’d been all day. She told me that a male nurse/CNA had tried to lift her by the neck that morning. Instead of the usual scoop under her entire neck used to help her sit up, he grasped her neck on each side and didn’t fully support the middle of her neck – at the top of her spine – and it had hurt.
When she reported this to staff that morning, they put her on bed rest for the entire day – changing diapers, serving meals in bed etc.
When I was leaving that evening I asked at the nursing station as to why she was on bedrest all day, the nurse (no name tag) checked her computer and she replied
“Nope nothing about bedrest. Nothing about her neck hurting – only that she “refused” exercise.”
I clarified “Nothing in her chart about her neck hurting or bedrest?”
The nurse replied “no.”
When I asked Helen about exercise the next day she told me she had been “too weak.” She had NOT “refused” exercise – she had been too weak!
I was appalled. They didn’t take her out for exercise for days, then chose to try to get her up for exercise the day after they’d kept her in bed all day, which had weakened her. I later learned that Helen expressing she was too weak to walk should have been reported to her doctor as a change in condition. None of this was included in her record.
(The strict federal and state rights include a patient’s to right to refuse care. The regulations also require skilled nursing facilities to report a change in the condition of a patient to their doctor right away. As Helen was typically up and about in her wheelchair several times a day, the record, in my opinion, incorrectly reflected a refusal of care, but should have reflected a change in condition and reported to her doctor. This is significant because this skilled nursing facility spent three years appealing a Medicare finding and substantial monetary fine, in another Patient case, blaming a severe injury of a 92 year-old resident on the elderly patient because she had the right to refuse assistance. The Medicare Administrative Law Judge (ALJ) stated “Thus, a refusal of treatment by a resident is not a free pass for the facility to avoid providing the care specified in the care plan.” The ALJ found against the Gardens in this case in 2022. One year later the facility appears to again be blaming the patient for her experience of subpar care instead of reporting to her doctor of her change to a weakened condition.)
[There are strict state and federal guidelines that prohibit physical or chemical restraints in nursing facilities. Penalties include costly fInes or loss of licensure. The loophole exists: the law does not recognize that staff refusal assist a patient, who requires assistance, to leave her bed as an unlawful restraint. ]
_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
Allegation #11, 9//21, 2023
I visited Helen first thing in the morning and helped her into a wheelchair so she could get out of bed. Later that day they got her up to walk but she could only take five steps and couldn’t take more than five steps to get back to her bed. She didn’t have the strength.
Allegation #12, 9/22/2023
Helen overheard staff talking outside her room that they no longer wanted to give her showers, but instead would bathe her in bed. She firmly told them she didn’t care about the future but wanted a shower now.The staff relented and gave her a shower.
(At minimum, standing in the hallway discussing Helen’s care plan that others could hear was a HIPAA violation.)
[“In-person discussions about patients: Casual discussions about patients violate HIPAA when they aren’t related to necessary treatment information and when they happen within earshot of employees and other patients, that aren’t essential to that treatment. Collaborations to treat a patient are acceptable but make sure they happen privately.”]
_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
Allegation # 13, In closing, I wrote:
More generally, staff has turned Helen’s visitors away, turned off the ringer on her phone – all without telling her. It left her wondering where all her friends were. This type of action left her feeling very isolated. Please don’t hesitate to call me.
X_ L&C was not able to validate the complaint allegation through direct observation, interviews, and/or review of documents. In addition, no other unrelated violations of regulations were observed.
The LACDPH staff never contacted me to interview me about the complaint and documentation I attached to the complaint.
I informed the Supervisor (I had first spoken with) that something was very wrong. I told him I wanted the “Unsubstantiated” sent to me in writing. I also told him I was going to the LA Times with this story. Suddenly, the next email I received had many recipients included in the thread, including staff at the California Department Of Public Health – the agency that contracts with LACDPH to investigate for the State and Medicare and sets the required policies and procedures that must be followed.
Here is what remains of Helen’s complaint that is available to the public; reduced to generic categories:
| ALLEGATION CATEGORY | ALLEGATION SUB CATEGORY | |
|---|---|---|
| Quality of Care/Treatment | Resident Safety | Unsubstantiated |
| Quality of Care/Treatment | Resident Dressed Improperly | Unsubstantiated |
| Resident/Patient/Client Rights | Other | Unsubstantiated |
| Resident/Patient/Client Rights | Other | Unsubstantiated |
| Resident/Patient/Client Rights | Other | Unsubstantiated |
| Resident/Patient/Client Rights | Other | Unsubstantiated |
| Quality of Care/Treatment | Res Meds Not Given According To Phys Instructions | Unsubstantiated |
| Resident/Patient/Client Rights | Resident Not Treated with Dignity/Respect | Unsubstantiated |
| Quality of Care/Treatment | Resident Is Over Sedated | Unsubstantiated |
| Quality of Care/Treatment | Resident Safety | Unsubstantiated |
| Quality of Care/Treatment | Call Bell Not Answered Timely Manner By Staff | Unsubstantiated |
| Resident/Patient/Client Rights | Other | Unsubstantiated |
| Quality of Care/Treatment | Other | Unsubstantiated |
Here is what remains of five years of ALL complaints made by concerned members of the public about the treatment and care received by their elderly loved ones in the facility where Helen lived:
| ALLEGATION CATEGORY | ALLEGATION SUB CATEGORY | INVESTIGATION FINDINGS | |
|---|---|---|---|
| 2024 | Resident/Patient/Client Abuse | Sexual | Unsubstantiated |
| 2023 | Infection Control | COVID19 — Noncompliance | Unsubstantiated |
| 2023 | Infection Control | PPE: Inadequate Supply/Improper Use | Unsubstantiated |
| 2023 | Quality of Care/Treatment | Resident Safety | Unsubstantiated |
| 2023 | Quality of Care/Treatment | Resident Dressed Improperly | Unsubstantiated |
| 2023 | Resident/Patient/Client Rights | Other | Unsubstantiated |
| 2023 | Resident/Patient/Client Rights | Other | Unsubstantiated |
| 2023 | Resident/Patient/Client Rights | Other | Unsubstantiated |
| 2023 | Resident/Patient/Client Rights | Other | Unsubstantiated |
| 2023 | Quality of Care/Treatment | Res Meds Not Given According To Phys Instructions | Unsubstantiated |
| 2023 | Resident/Patient/Client Rights | Resident Not Treated with Dignity/Respect | Unsubstantiated |
| 2023 | Quality of Care/Treatment | Resident Is Over Sedated | Unsubstantiated |
| 2023 | Quality of Care/Treatment | Resident Safety | Unsubstantiated |
| 2023 | Quality of Care/Treatment | Call Bell Not Answered Timely Manner By Staff | Unsubstantiated |
| 2023 | Resident/Patient/Client Rights | Other | Unsubstantiated |
| 2023 | Quality of Care/Treatment | Other | Unsubstantiated |
| 2022 | Infection Control | PPE: Inadequate Supply/Improper Use | No deficiencies noted |
| 2022 | Infection Control | COVID19 — Noncompliance | No deficiencies noted |
| 2022 | Death – General | Substantiated without deficiencies | |
| 2022 | Infection Control | COVID19 — Noncompliance | Unsubstantiated |
| 2022 | Resident/Patient/Client Rights | Other | Substantiated without deficiencies |
| 2022 | Admission, Transfer & Discharge Rights | Substantiated without deficiencies | |
| 2022 | Infection Control | COVID19 — Noncompliance | Unsubstantiated |
| 2022 | Infection Control | PPE: Inadequate Supply/Improper Use | Unsubstantiated |
| 2022 | Quality of Care/Treatment | Facility Staffing | Unsubstantiated |
| 2022 | Infection Control | COVID19 — Noncompliance | Unsubstantiated |
| 2022 | Infection Control | PPE: Inadequate Supply/Improper Use | Unsubstantiated |
| 2021 | Quality of Care/Treatment | Resident Safety/Falls | No deficiencies noted |
Not a single “substantiated with deficiencies” complaint with corrective action required, including Helen’s complaint.
Medicare uses California Department of Public Health investigation (called “survey”) findings to assign a star rating to nursing homes. It’s based on Los Angeles County Public Health FINDINGS. Los Angeles County Public Health finds complaints unsubstantiated – as it has for all of the Gardens complaints over the past five years (except a death which was Substantiated with no state or federal deficiencies.) This includes the very detailed and documented complaint about Helen’s care, but the Gardens retains its 5 star Medicare rating, based on LACDPH complaint findings.
To further complicate Helen’s situation, I felt obligated to let her adult children know that I had filed a complaint – and received a non-interested response:
A week later I emailed a copy of the complaint with the documentation to Helen’s daughter, and received no response.
Next week: Problems about the way LACDPH investigates complaints from the public about skilled nursing facilities have been known issue to the media, elected officials, and Medicare, for over 12 years!

