Helen just wanted to die. She couldn’t understand why she was still alive. By this time I had asked the social worker if there was a handout that explained how things “worked” in the facility- that is, meals, bathing, bedtime, mail…. Finally Helen was given a slim binder with some information. She was so relieved as she read through it. I later learned that legally Helen was legally entitled to this information as well as a copy of her state and federal rights at the time she had moved to the skilled nursing facility;
Basic Nursing Home Patient Rights & the California Residents’ Bill of Rights:
- Right to Dignity, Quality of Care, and Quality of Life
- Right to a Home-Like Living Environment
- Right to Make Health Care Decisions and decisions about her care plan,
- Right to know what medication she was be given and the purpose of the medication
- Right to Autonomy
- Right to chose what time to eat
- Right to choose her bedtime,
- Right to refuse care,
- Right to Privacy, Confidentiality, Visitors, and Communications
- The right to file a complaint.
Additionally, the American Medical Association Code of Ethics states:
“Respect for patient autonomy is central to professional ethics and physicians should involve patients in health care decisions commensurate with the patient’s decision-making capacity. Even when a medical condition or disorder impairs a patient’s decision-making capacity, the patient may still be able to participate in some aspects of decision making. Physicians should engage patients whose capacity is impaired in decisions involving their own care to the greatest extent possible, including when the patient has previously designated a surrogate to make decisions on his or her behalf.”
Unfortunately it would be another few weeks before I would learn about Helen’s legal rights. I did not learn about the AMA Code of Ethics until I wrote this blog. Meantime, Helen was suffering. She nicknamed one of her nurses “cold fish.” This woman was probably one of the most offensive of the staff. She’d demand, when Helen requested assistance using the restroom in the evening, that Helen decide if she then wanted to go to bed for the night. Helen was tired and it took her a minute to answer the question. When it took more than a few seconds, Nurse Cold Fish would walk out of the room, let me know what you decide – incredulously leaving her to pee in her diapers! Another time Helen complained of burning when she urinated. I asked for the nurse. Nurse Cold Fish came into Helen’s room, and when she heard Helen’s concern, she began arguing with her. You were offered a urine test on Friday and refused it! She raised her voice and repeated her words, this time leaning forward, towering over Helen, and pounding her finger on Helen’s overbed hospital table. I took a deep breath and interrupted. Is there any reason she cannot have a urine test now? I’ll contact the doctor, Nurse Cold Fish shouted over her shoulder as she exited Helen’s room. Three days later I checked with Helen and no urine sample had been collected, but she said the burning sensation was gone. I just took a deep breath and shook my head. Helen felt better and that’s what mattered. But she was also slipping into a major depression. She cried and just wanted to die. I asked her to text her doctor:
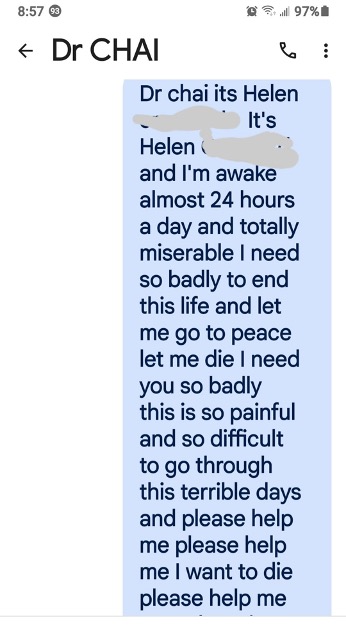
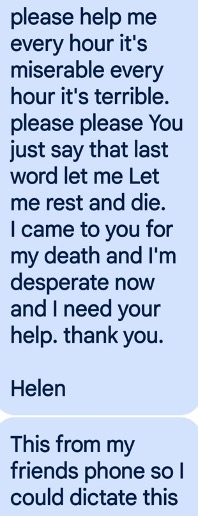
The doctor immediately ordered antidepressants and a sleeping pill. Helen began sleeping better with the pill and feeling better with the antidepressant. But that didn’t last long because Nurse Cold Fish began withholding her sleeping pill for several hours – because otherwise Helen “would wake up too early.” One afternoon I arrived around 6pm for my daily visit with Helen until she fell asleep for the night. We had a routine, we visited and chatted, and once she had her evening routine – restroom, pajamas, teeth brushed, medications, lip balm for her dry lips, and eye drops for her dry eyes – and a sleeping pill – we’d listen to classical music – she loved Beethoven. She would close her eyes as I massaged her swollen ankles and feet – she called them her elephant feet – until she fell asleep. I would carefully remove her hearing aids, tidy up her hospital table – throwing away the days trash, placing her reading material back on the clear filing trays we used to organize her table with things she needed easy access to – her glasses and cell phone, magazines, and a fresh cup of water. I was spending two to three hours a day with Helen, seven days a week; – visiting and watching over her. But this particular day was very different. As I walked into her room she was very upset. She exclaimed that she had asked for her sleeping pill at 4 pm and Nurse Cold Fish had told her she had to wait until 7 pm. Helen was unhappy and kept watching the clock on the wall as its hands ticked forward a minute at time. Finally seven o’clock! Helen grabbed her call button and pressed it. Nurse Cold Fish came in and said No you have to wait until 9 pm – Otherwise you will wake up too early. She also told Helen she would not give her her sleeping pill until I had left the room. Helen was upset. She had waited hours for her sleeping pill, but now she’d have to wait two more hours! She was totally dependent on the staff – for assistance to get out of bed, assistance to get into her wheelchair, assistance to use the restroom, assistance to receive her sleeping pill. She sent the message to Dr. Chai about wanting to die. Helen eyes were glued to the clock as the minutes ticked by. At nine o’clock Helen rushed me out of the room. I immediately left, but I waited down the hall to ensure that Nurse Cold Fish followed through with what she had promised. Fifteen minutes passed before Nurse Cold Fish appeared and entered Helen’s room. When the nurse left the room, I went home satisfied that Helen was taken care of for the night. But all was not well! The next morning Helen told me that when Nurse Cold Fish came back, she was late and that she had confessed to Helen that she had not been giving her a sleeping pill each night – that she had been giving her something else! No wonder Helen wasn’t sleeping well! Apparently when the doctor had received Helen’s text telling him she just wanted to die, he had called the facility because they had not advised him of her severe depression or her problems sleeping! He had made the appropriate prescriptions, and apparently told the nurse to update Helen with accurate information about her care and medications. Thus Nurse Cold Fish’s admission to Helen. What a chaotic place this was! No wonder Helen was so anxious and depressed!
A week later, I sat with Helen. Her mood was improving as she began to respond to the antidepressant medication Dr. Chai had prescribed. She still wanted to die – I’m 100 years old and have lived a good life. Why do I wake up? I talked to her about her care options:
- Regular treatment to keep her alive.
No, I don’t want that.
- Palliative care to keep her comfortable with possible curative care.
Maybe.
- Hospice care.
Yes, that’s what I want.
- End of life option.
No. I can’t do that.
As soon as Helen’s daughter-in-law learned that Helen wanted hospice she started calling local hospices til she found “the right one.” Two days later, the hospice intake nurse showed up to speak with Helen. Helen had told her daughter-in-law that she – Helen – was making her own decisions. I listened as he explained hospice to Helen. ….(and) I could have just given you a pain pill and you could be smiling and laughing and telling me you are in great pain and want more pain pills, and I can give them to you.
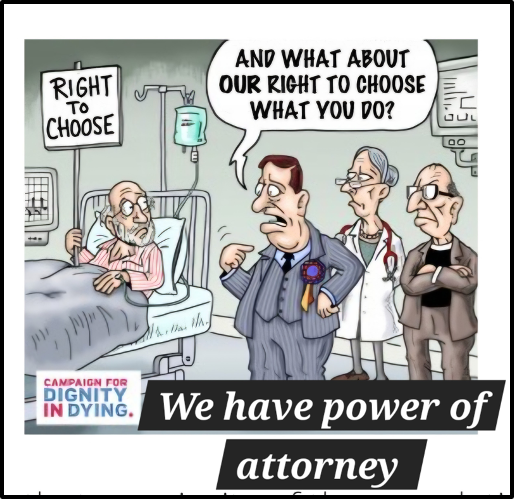
I thought his comment about pain medication was odd, but he quickly said So now we just need the signed paperwork that your family is faxing to us. I suggested he call and verify the paperwork would be faxed today. He called and Helen’s daughter-in-law picked up. She was on speaker and the first words put of her mouth were “She wants control.” Her tone was contemptuous – as if there was something wrong with Helen wanting to make decisions. He asked about the paperwork again and she responded “She wants control” – emphasizing the word control. My chest tightened – were they going to refuse to sign the paperwork since Helen wanted some control over her care plan? I whispered to the hospice nurse Ask if they can fax the signed paperwork by tonight. In response to his question he received a curt Yes. The signed paperwork arrived within the hour. I later asked Helen if she had named her daughter-in-law as power of attorney. No. Only my son and daughter. I asked my own attorney if those with power of attorney could delegate this role to someone else. The answer was No.
Her daughter-in-law was livid when she learned I told Helen that legally they cannot delegate their decision-making authority to anyone else – including her.
Next week: Hospice care begins, but Helen’s mis-treatment/abuse by the nursing facility staff worsens – and, in desperation, I call Adult Protective Services.

