Friends and neighbors helped Helen set up her new forever home. Her daughter and son were noticeably missing. She was downsizing from an 800 square foot, one bedroom home to a 140 square foot room with a private half-bathroom. Communal assisted showers and a bathtub were just down the hall. This meant we couldn’t move all her furniture into her new room, but we made it as beautiful and pleasant as possible.
Fresh sunflowers greeted her every morning, a sunflower-colored lightweight blanket served double duty – a pop of color on her bed that also kept the chill away. She looked out into a courtyard exploding with roses, tulips, geraniums where finches and hummingbirds darted around, sipping from bird feeders.
Sadly, though, Helen’s son and daughter, both in their sixties, were noticeably missing. Yet, when she lived in her one-bedroom home, her daughter visited her twice a month and often spent the entire day with her. Her son – her golden child – only seemed to visit on Christmas, Easter and Mother’s Day. He also controlled her money, which was “invested” in his business ventures. When Helen moved into her tiny room, her daughter’s visits shrank to twice a month for about an hour or two a visit.
Helen struggled desperately to adjust to her new routine, but no one had bothered explaining it to her. When did she eat? How would she receive her mail? When would she have a shower? Details like this, which most of us don’t even think about when we’re going about our lives, triggered debilitating anxiety in Helen.
Despite the efforts of friends and neighbors to cheer her up, she wanted to die. When she expressed her fears and unhappiness to her daughter and daughter-in-law, they not only lacked compassion and understanding, they were dismissive. You’re being well taken care of, they insisted. You need to adjust to your new routine. You’re fine.
I recognized that Helen had lived more than a century and understood her feelings that she was done and wanted to die. In our evening chats over the years, we had chatted about end of life options.
Meanwhile, the CNAs scurried in and out of her room. Time for a bath, Helen. Or Time for lunch. Or someone from the kitchen would drop by with a tray of ice cream. A nurse would arrive and announce it was time for her medication, give it to her, and then hurry on out. No one took the time to explain anything to her. She didn’t have any idea what her medication was for or why she was being treated with it. When she asked, the nurse told her she didn’t have time to explain and would hurry out. This was 180° from what she had experienced when she was temporarily in the facility.
Now when Helen pressed her call button and the CNAs ran into her room to find out what she needed, they turned off the call light and told her they would be back. But they never stated when they would be back – five minutes? Ten minutes? Thirty minutes?– which was a major violation of her rights. Helen had to press her call button every 30 minutes until she received assistance for something like assistance to use the toilet. I later learned that six months earlier, this facility was written up for not answering the call button in a timely manner. My belief now is they started “answering” by turning the call button off as if they had taken care of the matter when they had not. They were gaming the system. This is really critical because a later post will reveal that a complaint investigation about the staff turning the call light off and telling Helen they would be back, falsified the record by categorizing it as not answering the call button in a timely way and found it “unsubstantiated.” Of course it was unsubstantiated! Technically the staff answered the call request within five minutes – but only to turn it off – not to provide assistance for a bedridden patient.
Just think about that for a moment. Animals in shelters are treated more compassionately. Within a month, Helen was asking neighbors who visited her to find me and ask if I could visit her right away. She also left me a voicemail:
it’s Helen. And as you know, the girls are here. and I would love to talk to you. I’d love to have you meet them. But everything is strange and they’re going to come over about 2:00 this afternoon at the gardens. So that will cover something and I apologize. And please don’t please don’t leave me. Bye.”
With the assistance of The Garden’s social worker, Helen and I signed paperwork where she appointed me as her patient advocate. The social worker signed as the witness. The facility’s patient advocate program stated:
“The patient advocate can be authorized to access medical records and provide immediate information.”
However, when I requested a copy of Helen’s patient rights and her signature that she had received a copy – which I later learned by law the facility was required to give her – The Gardens refused to provide me with the information. I later learned that the facility’s staff were suddenly contacting families of other resident patients, asking them to sign forms that had never been signed – but should have been at time of admission. One family explained that they were asked to fill out a list of their mother’s belongings as a personal property inventory, a signature that they had received a copy of the Gardens’ policy regarding personal property, a signature on a paper acknowledging their mother had received a copy of her patient Bill of Rights etc. Their mother had been admitted years ago and they couldn’t recall what she had received, so they just signed the documents attesting that they had.
Meanwhile, her daughter went on a European vacation, her son didn’t visit much less call her. Helen had a strained relationship with his wife, her daughter-in-law. Out of sight, out of mind, seemed to be their operating procedure. Thoughtless? Cruel? Absolutely. But even worse, is that to Helen it seemed as if she was already dead.
Helen continued to try to advocate for herself:
- What are all these medications you’re giving me?” I asked for a print out for Helen. The nurse refused and instead scratched the names of different medications on a piece of paper, flashed it in front of Helen, then spun around leaving the room taking the paper with her.
- Helen wondered why her friends, who would visit after lunch throughout the afternoon weren’t stopping by anymore. What she did not know was that the nursing staff had posted a sign outside her door “No Visitors 2 – 4 pm.” They never told her about this sign. They had increased her isolation which added to her transfer trauma and I later learned it was a violation of her rights to deny visitors during regular day time/early evening hours.
- Helen would push the call button when she needed rest room assistance. The CNA would run into the room, ask what she wanted, turn the call light off and tell Helen she would be back. After 30 minutes of waiting Helen would push the call button again. The CNA would run into the room, hear Helen ask for rest room assistance, turn the call button off, spin and leave the room telling her she’d be back – leaving Helen sitting in now urine soaked diapers. I was dumbfounded. Sometimes I’d walk down to the nurses station to find CNAs sitting in the family room chatting, eating and scrolling on their phones. I’d ask if someone would please help Helen now, and someone would get up and help finally.
- Helen didn’t know how bedtime worked. We asked and were told “just ring the call button when she was ready for her bedtime routine – toilet use, brush teeth, wash her face, change into a nightgown, helped into bed and given a sleeping pill.” However, when she asked for help with her bedtime routine, it was the same thing – a CNA would run in, turn off the call light, leave while telling her she’d be back – then repeat – leaving Helen often waiting over an hour for assistance. I started spending every evening with Helen, chatting, listening to music, overseeing that her bedtime routine was taken care of and staying with her until she fell asleep. The staff was very lax about keeping her feet elevated during the day, so by night her ankles had swollen to the size that Helen referred to her “elephant feet.” I massaged her swollen feet for 30 to 60 minutes each evening, and each night had to ask for her eye drops for her dry eyes that the doctor had ordered.
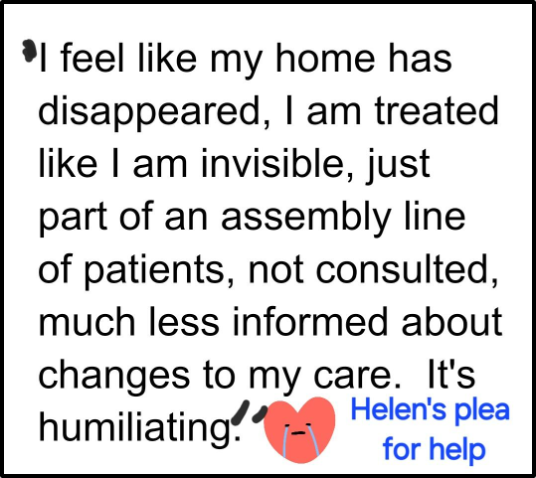
Helen just wanted to die. She felt like her home had disappeared, that she was just invisible – part of an assembly line, she felt humiliated. She asked for a meeting with the social worker and some of her friends to talk about her experience so others would know what was going on. Instead the social worker came to her room with another woman whom she didn’t identify or introduce, who stood over her with a clipboard taking notes. Helen talked about her concerns and finally said “I feel like I’m being interrogated, I feel intimidated, and I want to stop.” The social worker pleasantly assured her they could stop and asked “Do we still need to have that meeting?” Helen said “no.” The meeting she wanted had not happened. She had wanted to have the meeting, with witnesses, so things would change so that no one else would go through what she was going through. She was exhausted and I wanted her to rest, so I didn’t bring it up. I would later realize, this “listening and then do nothing” was the “standard operating procedure” that administrators at the Gardens used to get rid of concerns – “Listen, make ‘em feel good, and they”ll go away” (and probably forget all about their concerns – after all these are old people.)
Next week Helen decides her time has come and talks about “Dignity with Death” with an unexpected response by her daughter-in-law, daughter and son.
Tell Your Story! Please share it in the comment section below and include the state where the incidents occurred.


[…] I reflect back on my dear friend Helen, the care I observed her receiving was that of assisted living. When Helen had 100 days of Medicare […]