An Exposè: When is a 5 Star Nursing Home not a 5 Star Facility?

After billions of federal Medicare dollars paid to Los Angeles Department of Public Health by the California Department of Public Health, for over 12 years of egregiously misleading, subpar and falsified investigation results, Los Angeles County Public Health Department’s contract is up for renewal next year. Enough is Enough! Do NOT Renew It! PROTECT OUR ELDERS FROM ABUSE AND NEGLECT – and falsified report findings that cover it up. Helen’s wish was that no one else would go through what she went through.
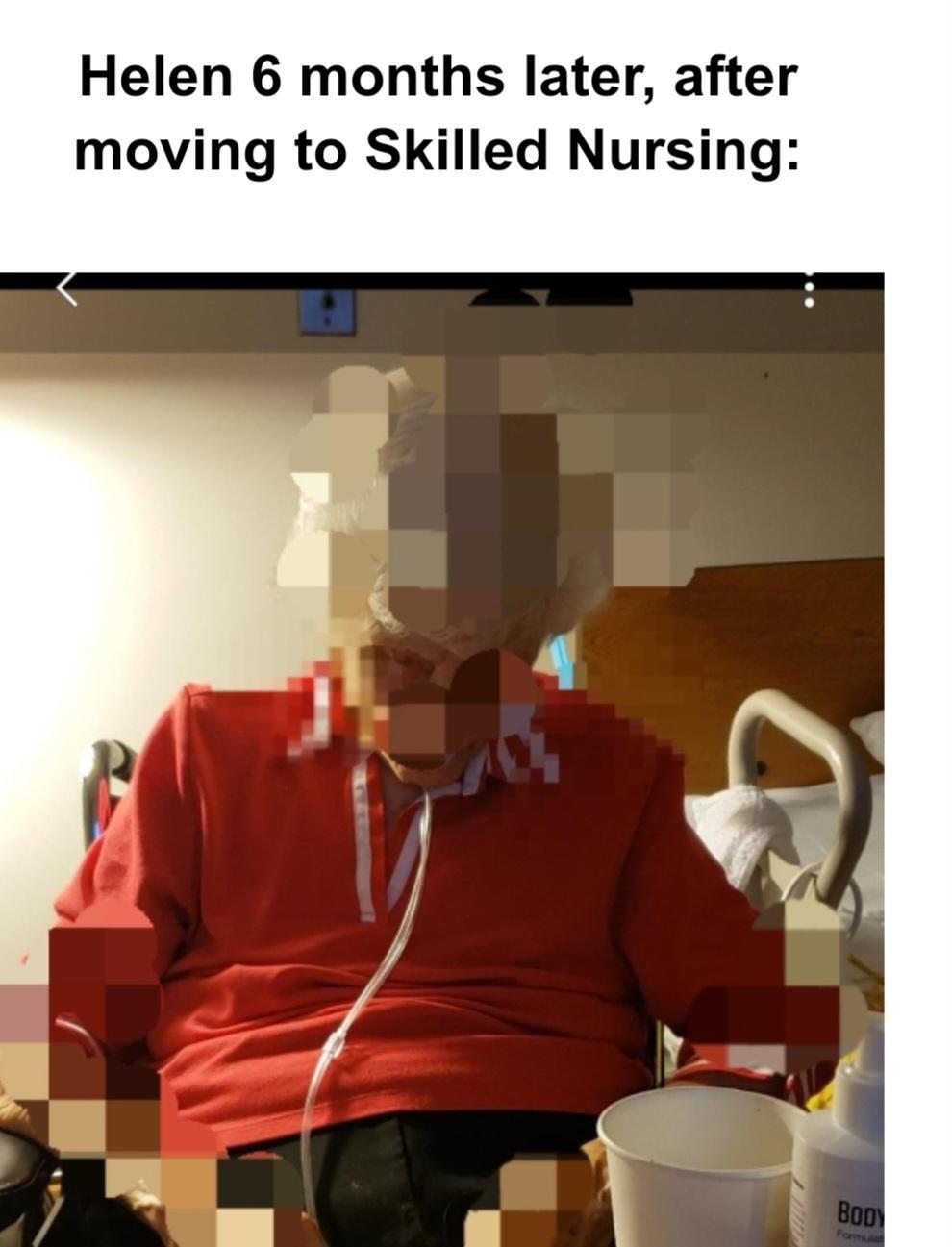
My dear friend Helen, at 100.5 years old, was transferred from her home in independent living, where she had resided for 22 years – the last 10 years as a widow, to the Skilled Nursing Facility (SNF) in her Life Plan [aka Continuing Care Retirement (CCRC)] Community.
So many things went wrong for Helen that almost overnight, she went from being vibrant, poised, confident, and self-controlled to terror-stricken, anxious, and distraught. She was treated terribly by the staff, as if she was nothing more than an annoying object. She felt humiliated. She made me promise to take notes and write about her treatment so that no one else would go through the horror that she was experiencing. This blog-story includes the fulfillment of that promise.
California law requires that each and every person admitted to a nursing facility in the state must be provided with a printout of their rights – i.e. be treated with dignity, be included in their care and treatment planning and decisions, choose their bedtime, etc. The law requires that the patient must be provided a copy of their rights at the time of EACH admission and they must be signed and dated, acknowledging that they received the document. Her rights are her roadmap for the standards of care she is legally entitled to. None of this was done for Helen – or for others.. If she had received a print out of her rights, it would have given us something to refer to when attempting to address the issues with staff.
Lacking this information about patient rights, I later, after walking home in tears after one evening visit, and in desperation, called adult protective services to report elder abuse. I was told to call one agency after another – because the nursing home was located within “congregant living.” No one seemed to know who I should call!
Four months after her 100th birthday, Helen was temporarily moved to skilled nursing for back pain – pain which became so extreme her family approved hospice so that she could be administered morphine. She was so drugged she could barely speak – and remarkably, she was aware of it! She was able to describe, slowly, as she struggled to find the right words, that she “didn’t feel like herself – that everything was floating.” She wondered if she’d had a stroke – that’s how cognitively functional she was while heavily sedated with morphine, at 100 years old!
In Boomer language, she was stoned almost out of her mind, but she knew something was wrong! Through her morphine-induced brain fog she could describe it and state that she didn’t like it. Helen was a senior known as a super-ager – “…people in their 70s and 80s (90s+) who have the mental or physical capability of their decades -younger counterparts. They may approach tasks as a challenge they can succeed at, in contrast to typical other older adults who may give up.” Nursing facilities staff do well with most patients because they give up and adapt – and do not do well with patients who have their critical thinking skills intact. MORE ON THIS in a LATER POST
I later realized that these superagers are intentionally subjected to having their control taken away – not allowed to choose their bed time, waiting long periods of time before they are taken to the restroom, not included in their care planning etc. Being subject to such enormous loss of control subjects these patients to severe transfer trauma with symptoms that may lead to a misdiagnosis of Dementia, or “Fluid” awareness and cognitive abilities – leading to staff dismissing much of what the elderly patient says. For example, I was present at a meeting between Helen and the facility social worker. Helen was telling the social worker that she had visited the independent living business center the prior day with one of her friends, and checked for her mail. She found four cards addressed to her scattered across the floor of the mail center – waving her hand to demonstrate how her mail was strewn across the floor. The social worker later told me that Helen’s mental capacity was “fluid,” – citing how Helen had waved her hand to indicate that her mail was laying on the floor of her small room. I corrected her and stated that Helen was demonstrating how she found her mail on the floor of the business center. Helen was telling her that she wanted her mail delivered to her to the nursing facility. The social worker heard her words as a delusion and simply placated her and did nothing. I would later begin to wonder if retirement communities in general, not just skilled nursing facilities, count on age-related loss of stamina and cognitive decline, to provide and cover up subpar care and discrimination. Hiring a social worker with only an undergraduate degree and no supervised training compounds these problems.
After two weeks, they took Helen off the 15 mg doses of morphine that had been administered 2x a day – i.e., cold turkey. She was given a less potent pain medication. She asked for it often. Her RN only denied her request if four hours had not passed since the last dose. The CNAs – certified nursing assistants would answer her call button within five minutes and take care of what she needed right away. The CNAs stopped by her room just to say “hi” and would stay a few minutes and kid her about Don. He was a widower who also visited her every day, affectionately laughing with her, and the CNAs kidded her about having a boyfriend. Her friends came by to visit and read to her. She was still needing pain medication but felt so valued and cared for – very much like those of us who lived in independent living. We had all received caring treatment in independent living — Helen in her 22 years at the Gardens, and me in my five years. Given our experience in independent living, it was a reasonable expectation this quality care would continue.
Helen began to seriously consider moving to the skilled nursing facility permanently. The powers that be were strongly recommending she make this move to a higher level of care – and skip the assisted living level of care. She was treated well and could easily be visited by her friends – the very reason we had all moved to the Gardens. It seemed that all was well. And it was….
– ….. but not for long.
Years earlier, all of us had been sold on The Gardens in the introductory marketing pitch presentation – The Road Ahead. Helen was artistic and she and I began talking about how she might decorate her bathroom – to transform it from institutional to home-like – the very essence of the Gardens ongoing marketing campaign to “Make Your Home Your Own.” It was ideal.
– or so we thought…. but we couldn’t have been more mistaken.
Next week “What Happened Next” – Helen gave up her apartment and moved into skilled nursing permanently, and everything began changing for her.
….But not the way we’d hope for…
Life went from good – to bad – to ugly…..Tell Your Story! Please share it in the comment section below and include the state where the incidents occurred.

